Masculinizing Hormone Therapy
The cornerstone of hormone therapy for trans men is testosterone. The goal of treatment is virilization – development of masculine secondary sexual characteristics.
Quick reference guide for masculinizing hormone therapy
-
Topics in this section:
- Hormonal agents
- Expected effects
- Risk mitigation
- Monitoring strategies
- Long-term preventive care
Hormonal agents
Testosterone
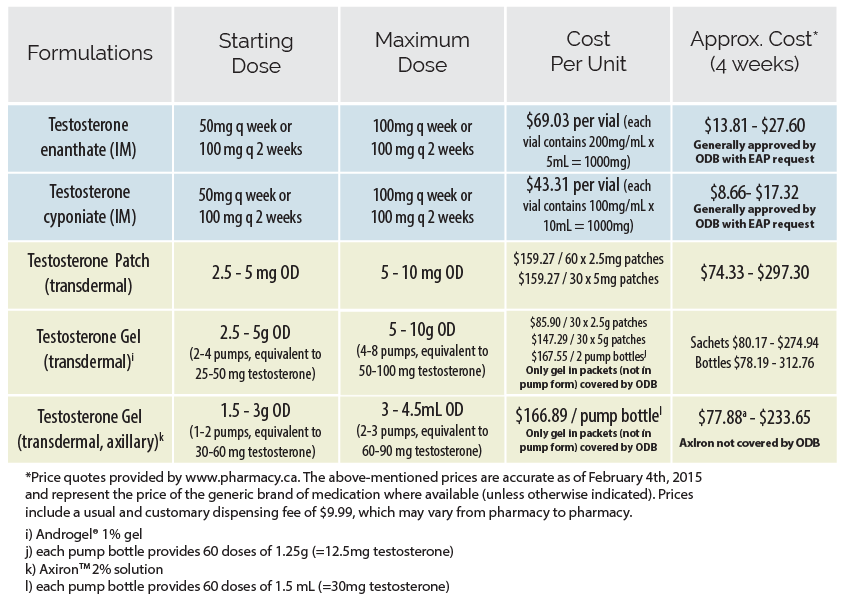
In Ontario, options for testosterone administration include injectable and transdermal preparations (patch or gel). Injectable formulations are most commonly used, both because of their superior efficacy and lower price.
View formulations, recommended doses and costs of testosterone
Expected effects
What to expect from a regimen consisting of testosterone
The degree and rate of physical effects is dependent on the dose and route of administration, as well as client-specific factors such as age, genetics, body habitus and lifestyle.
Desired androgenic effects of testosterone therapy include deepened voice, cessation of menses, clitoral growth, increased muscle mass, and hair growth in androgen dependent areas including facial hair. Typically, clients taking testosterone develop a male phenotype over a period of months to years. The timeframe of physiologic changes may be slightly slower with the use of transdermal preparations.
Effects and expected time course Download
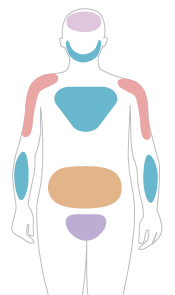
Hover over the coloured regions to view expected information on the reversibility, onset and maximum effects of physical changes
Skin changes
Skin oiliness and acne increases
- Reversibility:
- Reversible
- Expected onset:
- 1 - 6 months
- Expected max. effect:
- 1 - 2 years
Body and facial hair growth
Facial hair grows and body hair thickens.
- Reversibility:
- Irreversible
- Expected onset:
- 3 - 6 months
- Expected max. effect:
- 3 - 5 years
Scalp hair loss
Highly dependent on age and inheritance; may be minimal
- Reversibility:
- Irreversible
- Expected onset:
- > 12 months
- Expected max. effect:
- Variable
Deepening of voice
- Reversibility:
- Irreversible
- Expected onset:
- 3 - 12 months
- Expected max. effect:
- 1 - 2 years
Cessation of menses
- Reversibility:
- Reversible
- Expected onset:
- 2 - 6 months
Clitoral enlargement
- Reversibility:
- Irreversible
- Expected onset:
- 3 - 6 months
- Expected max. effect:
- 1 - 2 years
Vaginal atrophy
- Reversibility:
- Reversible
- Expected onset:
- 3 - 6 months
- Expected max. effect:
- 1 - 2 years
Increased muscle mass/strength
Significantly dependent on amount of exercise
- Reversibility:
- Reversible
- Expected onset:
- 6 - 12 months
- Expected max. effect:
- 2 - 5 years
Fat redistribution
Fat redistributes from buttock/hip/thigh regions to the abdomen and mid-section.
- Reversibility:
- Reversible
- Expected onset:
- 3 - 6 months
- Expected max. effect:
- 2 - 5 years
Risk mitigation
Absolute contraindications
- Pregnancy or breast feeding
- Active known androgen-sensitive cancer
- Unstable ischemic cardiovascular disease
- Active endometrial cancer
- Poorly controlled psychosis or acute homicidality
- Psychiatric conditions which limit the ability to provide informed consent
- Hypersensitivity to one of the components of the formulation
Precautions and risk mitigation Download
Several pre-existing medical conditions and risk factors may increase the risks associated with testosterone administration. When these are present, a careful evaluation of risks and benefits should be completed and fully discussed with the client.
Select area of concern below
Neurologic
| Risk factors | How to minimize risks |
|---|---|
| Migraines | Consider referral to neurology, consider daily migraine prophylaxis, consider transdermal route of administration |
| Androgen-sensitive epilepsy | Refer to neurology |
Endocrine
For more information on metabolic effects please read page 24 of the full Protocols.
| Risk factors | How to minimize risks |
|---|---|
| Uncontrolled diabetes | Identify and address barriers to optimal glycemic control, refer to dietician, encourage lifestyle modification, initiate antiglycemic agent(s), consider cardiac stress test, encourage deferral of testosterone until adequately controlled |
| Uncontrolled dyslipidemia | Identify and address barriers to optimal lipid control, refer to dietician, initiate antilipemic pharmacologic therapy, consider endocrinology referral, consider cardiac stress test, encourage deferral of testosterone until addressed |
Cardiovascular
For more information on cardiovascular disease please read page 24 of the full Protocols.
| Risk factors | How to minimize risks |
|---|---|
| Stable ischemic cardiovascular disease | Consider referral to cardiology, ensure optimal medical (including prophylactic anticoagulation) and/or surgical management as indicated, aggressive risk factor optimization, consider transdermal route of administration +/- lower dose |
| Uncontrolled high blood pressure | Identify and address barriers to optimal BP control, initiate antihypertensive(s) as needed, consider cardiac stress test, encourage deferral of testosterone until adequately controlled |
Hepatic
Elevation of liver enzymes may occur with testosterone therapy. For more information on cardiovascular disease please read page 25 of the full Protocols.
| Risk factor | How to minimize risks |
|---|---|
| Hepatic dysfunction | Dependent on etiology, e.g. minimize alcohol consumption, weight loss in NAFLD, consider referral to hepatology/GI |
Gynacologic
For more information on endometrial cancer please read page 25 of the full Protocols.
Sources
- Cattrall FR, Healy DL. Long-term metabolic, cardiovascular and neoplastic risks with polycystic ovary syndrome. Best Practice &smp; Research Clinical Obstetrics & Gynaecology. 2004; 18(5):803-812.
- Perrone AM, Cerpolini S, Maria Salfi NC, Ceccarelli C, De Giorgi LB, Formelli G, Meriggiola MC. Effect of Long-Term Testosterone Administration on the Endometrium of Female-to-Male (FtM) Transsexuals. The journal of sexual medicine. 2009; 6(11):3193-3200.
- Grynberg M, Fanchin R. Dubost G. Colau JC, Brémont-Weil C, Frydman R, Ayoubi JM. Histology of genital tract and breast tissue after long-term testosterone administration in a female-to-male transsexual population. Reproductive biomedicine online. 2010; 20(4):553-558.
- Feldman J and Safer J. 2009. Hormone Therapy in Adults: Suggested Revisions to the Sixth Version of the Standards of Care , Intl J of Transgenderism. 2009; 11(3)146-182, DOI: 10.1080/15532730903383757
| Risk factors | How to minimize risks |
|---|---|
| Inter-menstrual bleeding | Consider pelvic ultrasound (transvaginal if possible), consider gyne referral - especially if significant risk factors for endometrial cancer |
| Oligo-/amenorrhea | Consider pelvic ultrasound (transvaginal if possible), consider progesterone-induced menstrual bleed prior to testosterone initiation |
Hematologic
| Risk factors | How to minimize risks |
|---|---|
| Polycythemia | Refer to hematology, identify etiology and address contributing factors, consider low-dose ASA, strongly encourage deferral until adequately managed, consider transdermal route of administration, monitor RBCs/Hct closely. More information on this on page 25 of the full Protocols |
| History of deep vein thrombosis (DVT), pulmonary embolism (PE) or hypercoagulable state | Identify and minimize co-existent risk factors, monitor RBCs/Hct closely, consider transdermal route of administration |
Respiratory
| Risks/Precautions | How to minimize risks |
|---|---|
| Smoker | Encourage and support smoking cessation, offer NRT and/or bupropion/varenacline, or negotiate a decrease in smoking, consider cardiac stress test especially in the presence of additional risk factors, consider transdermal route of administration |
| Chronic respiratory disease that may be worsened by erythrocytosis/polycythemia | Consider referral to respirology, monitor RBCs/Hct closely, consider transdermal route of administration |
| Severe/uncontrolled sleep apnea | Initiate CPAP or oral device, encourage weight loss if overweight, consider uvulopalatoplasty, monitor for changes in CPAP pressure requirements. More information on page 25 of the full Protocols |
Monitoring strategies
Standard monitoring of estrogen administration should be employed at baseline, 1, 3, 6, and 12 months. This should include a functional inquiry, targeted physical exam, bloodwork, and health promotion/ disease prevention counselling.
Testosterone level may be the most useful test for monitoring in trans women; for many clients, the goal will be to achieve the suppression of testosterone into the female range. That said, the client may have clinically relevant results without total suppression of testosterone because of androgen blockade, which is not easily measured. Estradiol levels are of variable utility in monitoring feminizing therapy given the wide cyclical variation in cis women. Most clients attain considerable feminization at estradiol levels between 200-500 pmol/L. According to the Endocrine Society Guidelines, serum estradiol levels should not exceed the mean daily level for cis women (approximately 700 pmol/L).
Hormone Monitoring Summary Download
Click on one of the tabs to find out standard monitoring suggestions at baseline, 1, 3 and 6 months.
Review with client:
-
Contraindications and precautions
-
Old records
-
Mental health
- Screen for depressive symptoms (including suicidality) and anxiety disorders
- Inquire re: symptoms of hypomania, mania, or psychotic symptoms
- Inquire re: current level of gender dysphoria and body image
- Screen for disordered eating
- Assess client interest in surgical treatments if not accessed
- Inquire re: libido/changes in libido
-
Education / Lifestyle Counselling
- Review healthy eating and general nutrition
- Adequate Calcium Intake – ensure a minimum intake of 1200 mg of Calcium daily (total: diet + supplements)
- Adequate Vitamin D – ensure 1000 IU of vitamin D daily
- Hormone Adherence – missed doses of testosterone will impact bone health if post-oophorectomy, while extra doses may lead to a host of problems associated with supraphysiologic levels
- Regular, moderate physical activity – weight-bearing exercise helps in osteoporosis prevention; to avoid tendon rupture, weight loads used in strength training should be increased gradually with an emphasis on repetitions and stretching
- Safe sex practices/STI counselling – trans men may be at high risk of STIs depending on behavioural factors; safer sex counselling and frequent screening (i.e. every 3 months) for those at risk is imperative (for client-centred handout materials, see Primed: The Back Pocket Guide for Trans Men and the Men Who Dig Them
- Potential for pregnancy/need for birth control – trans men on testosterone may become pregnant even if menstrual suppression has been achieved and should be counselled in this regard; given that testosterone is a teratogen, reliable birth control should be instituted where pregnancy is a risk based on sexual activity
- Smoking – cessation, stages of readiness, etc.
- Alcohol and other substances – inquire re: problematic use of substances including alcohol, cannabis, cocaine, opioids, hallucinogens, ketamine, ecstasy, and anabolic steroids; trans men should follow the safe drinking guidelines as for cis women (see Canada’s Low-risk Alcohol Drinking Guidelines)
-
Psychosocial
- An effort should be made to assess the impact of transition/trans identity on employment, housing, family, relationships, and economic wellbeing
- Social Supports – specific attention should be given to assessing the extent of a client’s social supports, creating an opportunity to suggest additional resources if needed
- Name change/identification – assess client need/ desire to change name and/or gender marker on identification and offer support for this process (see template letters and RHO fact sheets in the resources section)
-
Health maintenance
- Immunization history
- STI screening, HIV risk assessment and screening
- TB skin test
Examinations/Investigations:
-
Pregnancy test prior to 1st injection
-
Full Physical Exam with PAP if indicated
- Follow cervical cancer screening guidelines as for ciswomen if the cervix is present. For more information see next section on long-term preventive care.
-
Measurements
- height, weight, waist & abdo circ.
-
EKG / cardiac stress test
- EKG for clients over 40
- EKG and cardiac stress test if client has additional risk factors
Bloodwork:
-
CBC
-
ALT/AST (if restricted in ordering OHIP-covered AST levels, ALT alone may be used to screen for liver dysfunction)
-
Fasting Glucose
-
LDL/HDL/TG
-
Testosterone (+/- Estradiol)
-
LH (Elevated LH post-gonadectomy may have implications regarding bone mineral density - See Full Protocols for Osteoporosis and BMD Screening)
Review with client:
-
Hormone effects
-
Cessation of menses
-
Mental health
- Screen for depressive symptoms (including suicidality) and anxiety disorders
- Inquire re: symptoms of hypomania, mania, or psychotic symptoms
- Inquire re: current level of gender dysphoria and body image
- Screen for disordered eating
- Assess client interest in surgical treatments if not accessed
- Inquire re: libido/changes in libido
-
Education / Lifestyle Counselling
- Review healthy eating and general nutrition
- Adequate Calcium Intake – ensure a minimum intake of 1200 mg of Calcium daily (total: diet + supplements)
- Adequate Vitamin D – ensure 1000 IU of vitamin D daily
- Hormone Adherence – missed doses of testosterone will impact bone health if post-oophorectomy, while extra doses may lead to a host of problems associated with supraphysiologic levels
- Regular, moderate physical activity – weight-bearing exercise helps in osteoporosis prevention; to avoid tendon rupture, weight loads used in strength training should be increased gradually with an emphasis on repetitions and stretching
- Safe sex practices/STI counselling – trans men may be at high risk of STIs depending on behavioural factors; safer sex counselling and frequent screening (i.e. every 3 months) for those at risk is imperative (for client-centred handout materials, see Primed: The Back Pocket Guide for Trans Men and the Men Who Dig Them
- Potential for pregnancy/need for birth control – trans men on testosterone may become pregnant even if menstrual suppression has been achieved and should be counselled in this regard; given that testosterone is a teratogen, reliable birth control should be instituted where pregnancy is a risk based on sexual activity
- Smoking – cessation, stages of readiness, etc.
- Alcohol and other substances – inquire re: problematic use of substances including alcohol, cannabis, cocaine, opioids, hallucinogens, ketamine, ecstasy, and anabolic steroids; trans men should follow the safe drinking guidelines as for cis women (see Canada’s Low-risk Alcohol Drinking Guidelines)
-
Psychosocial
- An effort should be made to assess the impact of transition/trans identity on employment, housing, family, relationships, and economic wellbeing
- Social Supports – specific attention should be given to assessing the extent of a client’s social supports, creating an opportunity to suggest additional resources if needed
- Name change/identification – assess client need/ desire to change name and/or gender marker on identification and offer support for this process (see template letters and RHO fact sheets in the resources section)
Examinations/Investigations:
-
Measurements
- blood pressure, weight, waist & abdo circ.
-
Abdominal exam including liver palpation
-
Immunizations
- Vaccinate for Hep A & B, Td and Pneumovax as indicated, Consider HPV vaccination series
Bloodwork:
-
CBC
-
ALT/AST (if restricted in ordering OHIP-covered AST levels, ALT alone may be used to screen for liver dysfunction)
-
Testosterone (+/- Estradiol)
Review with client:
-
Hormone effects
-
Cessation of menses
-
Mental health
- Screen for depressive symptoms (including suicidality) and anxiety disorders
- Inquire re: symptoms of hypomania, mania, or psychotic symptoms
- Inquire re: current level of gender dysphoria and body image
- Screen for disordered eating
- Assess client interest in surgical treatments if not accessed
- Inquire re: libido/changes in libido
-
Education / Lifestyle Counselling
- Review healthy eating and general nutrition
- Adequate Calcium Intake – ensure a minimum intake of 1200 mg of Calcium daily (total: diet + supplements)
- Adequate Vitamin D – ensure 1000 IU of vitamin D daily
- Hormone Adherence – missed doses of testosterone will impact bone health if post-oophorectomy, while extra doses may lead to a host of problems associated with supraphysiologic levels
- Regular, moderate physical activity – weight-bearing exercise helps in osteoporosis prevention; to avoid tendon rupture, weight loads used in strength training should be increased gradually with an emphasis on repetitions and stretching
- Safe sex practices/STI counselling – trans men may be at high risk of STIs depending on behavioural factors; safer sex counselling and frequent screening (i.e. every 3 months) for those at risk is imperative (for client-centred handout materials, see Primed: The Back Pocket Guide for Trans Men and the Men Who Dig Them
- Potential for pregnancy/need for birth control – trans men on testosterone may become pregnant even if menstrual suppression has been achieved and should be counselled in this regard; given that testosterone is a teratogen, reliable birth control should be instituted where pregnancy is a risk based on sexual activity
- Smoking – cessation, stages of readiness, etc.
- Alcohol and other substances – inquire re: problematic use of substances including alcohol, cannabis, cocaine, opioids, hallucinogens, ketamine, ecstasy, and anabolic steroids; trans men should follow the safe drinking guidelines as for cis women (see Canada’s Low-risk Alcohol Drinking Guidelines)
-
Psychosocial
- An effort should be made to assess the impact of transition/trans identity on employment, housing, family, relationships, and economic wellbeing
- Social Supports – specific attention should be given to assessing the extent of a client’s social supports, creating an opportunity to suggest additional resources if needed
- Name change/identification – assess client need/ desire to change name and/or gender marker on identification and offer support for this process (see template letters and RHO fact sheets in the resources section)
Examinations/Investigations:
-
Measurements
- blood pressure, weight, waist & abdo circ.
-
Abdominal exam including liver palpation
Bloodwork:
-
CBC
-
ALT/AST (if restricted in ordering OHIP-covered AST levels, ALT alone may be used to screen for liver dysfunction)
-
Testosterone (+/- Estradiol)
Review with client:
-
Hormone effects
-
Cessation of menses
-
Mental health
- Screen for depressive symptoms (including suicidality) and anxiety disorders
- Inquire re: symptoms of hypomania, mania, or psychotic symptoms
- Inquire re: current level of gender dysphoria and body image
- Screen for disordered eating
- Assess client interest in surgical treatments if not accessed
- Inquire re: libido/changes in libido
-
Education / Lifestyle Counselling
- Review healthy eating and general nutrition
- Adequate Calcium Intake – ensure a minimum intake of 1200 mg of Calcium daily (total: diet + supplements)
- Adequate Vitamin D – ensure 1000 IU of vitamin D daily
- Hormone Adherence – missed doses of testosterone will impact bone health if post-oophorectomy, while extra doses may lead to a host of problems associated with supraphysiologic levels
- Regular, moderate physical activity – weight-bearing exercise helps in osteoporosis prevention; to avoid tendon rupture, weight loads used in strength training should be increased gradually with an emphasis on repetitions and stretching
- Safe sex practices/STI counselling – trans men may be at high risk of STIs depending on behavioural factors; safer sex counselling and frequent screening (i.e. every 3 months) for those at risk is imperative (for client-centred handout materials, see Primed: The Back Pocket Guide for Trans Men and the Men Who Dig Them
- Potential for pregnancy/need for birth control – trans men on testosterone may become pregnant even if menstrual suppression has been achieved and should be counselled in this regard; given that testosterone is a teratogen, reliable birth control should be instituted where pregnancy is a risk based on sexual activity
- Smoking – cessation, stages of readiness, etc.
- Alcohol and other substances – inquire re: problematic use of substances including alcohol, cannabis, cocaine, opioids, hallucinogens, ketamine, ecstasy, and anabolic steroids; trans men should follow the safe drinking guidelines as for cis women (see Canada’s Low-risk Alcohol Drinking Guidelines)
-
Psychosocial
- An effort should be made to assess the impact of transition/trans identity on employment, housing, family, relationships, and economic wellbeing
- Social Supports – specific attention should be given to assessing the extent of a client’s social supports, creating an opportunity to suggest additional resources if needed
- Name change/identification – assess client need/ desire to change name and/or gender marker on identification and offer support for this process (see template letters and RHO fact sheets in the resources section)
Examinations/Investigations:
-
Measurements
- blood pressure, weight, waist & abdo circ.
-
Abdominal exam including liver palpation
Bloodwork:
-
CBC
-
ALT/AST (if restricted in ordering OHIP-covered AST levels, ALT alone may be used to screen for liver dysfunction)
-
Fasting Glucose
-
LDL/HDL/TG
-
Testosterone (+/- Estradiol)
-
LH (Elevated LH post-gonadectomy may have implications regarding bone mineral density - See Full Protocols for Osteoporosis and BMD Screening)
Long-term preventive care
Trans men maintained on masculinizing hormone therapy have unique preventive care needs and recommendations.
Long-term follow-up care of trans men on masculinizing hormone therapy should involve (at least) annual preventive care visits. An Adaptive Preventive Care Checklist with accompanying explanations for trans-specific recommendations can be accessed below.
-
Adapted Preventive Care Checklist for Trans Men
-
Accompanied Explanations for Trans-specific Recommendations
Preventive care screening procedures
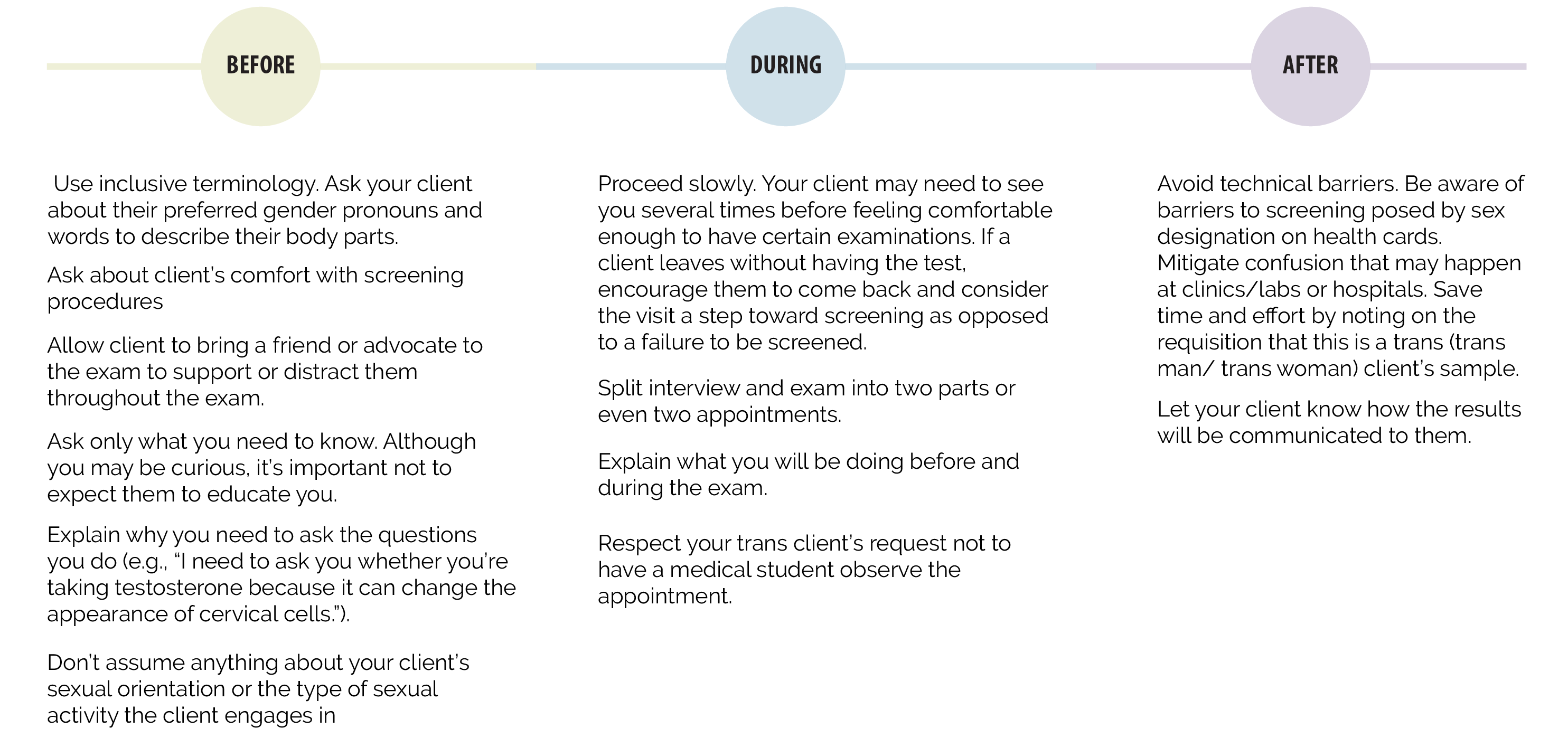
Physical examinations that involve intimate body parts are discomforting to anyone. While many trans people are comfortable with their bodies others may experience body dysphoria. Some may be very uncomfortable with physical examinations or be reluctant to acknowledge or touch their own genitals.
View tips on increasing client comfort before, during and after exams
Provide care based on organs present
It is best to base routine screening on the presence or absence of body parts. Sex assigned at birth and gender identity are separate things. Some women have pensises, some men have vaginas. Refrain from calling body parts ‘male’ or female’. Instead use technical terms or ask client what they prefer to call their body parts. Organs present should receive routine and preventive care.
Click on one of the tabs to find out routine care and screening suggestions.
Osteoporosis and Bone Mineral Density Screening
Indications for BMD screening
- Trans men at any age having undergone oophorectomy and having been off exogenous hormones for any significant length of time
- Client over 50 years old regardless of ovarian status if have taken testosterone for any significant length of time and have any other risk factors for osteoporosis
- Client over 50 years old with ovaries intact and 5-10+ years on testosterone
- Client over 50 years old post-oophorectomy and on testosterone over 5 years
- Client over 60 years old post-oophorectomy and on testosterone under 5 years
Breast/Chest exam
Recommendations for clients at average risk of developing breast cancer:

Risks for developing breast/chest cancer depend on:
- amount of tissue removed during top surgery
- personal risk factors and history
- whether the client has had his ovaries removed
- whether the client is taking testosterone and other hormone therapies. Some studies show that excess testosterone in the body can be converted to estrogen, increasing the risk of breast cancer.
- mammography may not be possible following a mastectomy in some cases. Breast ultrasound or MRI may be a preferable method of screening.
People at high risk may have:
- a genetic mutation that puts them at a higher risk for breast/chest cancer
- a parent, sibling or child who has a genetic mutation that puts them at a higher risk for breast/chest cancer
- a family history that indicates a lifetime risk of breast/chest cancer that is equal to or greater than 25% confirmed through genetic assessment
- received radiation therapy to the chest before 30 years of age as treatment for another cancer or condition (for example, Hodgkin’s disease)
- Some trans men may prefer to use the term chest over breast(s)
- For trans men who are male assigned on their health card, they will not be able to self-refer to Ontario Breast Screening Program. A requisition is required.
Colon cancer screening
Use the diagram below to find out when and what type of colon cancer screening is recommended.
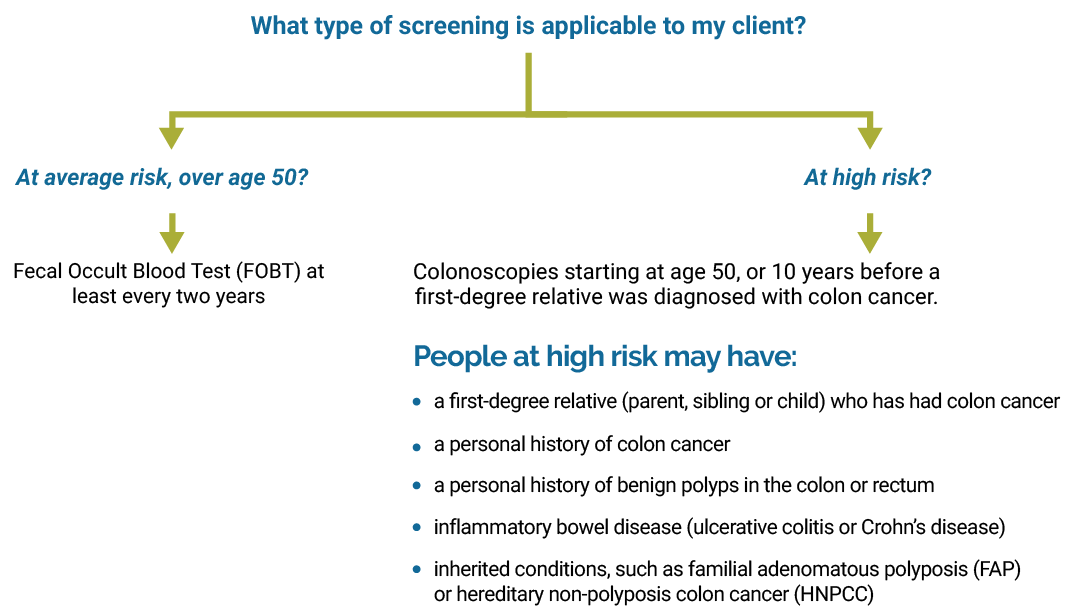
- Where possible, requisition the colonoscopy at a clinic or hospital with experience in and sensitivity training for LGBTQ populations. If you’re not sure, telephone the clinic in advance and speak to the manager or director to let them know that you are referring a trans client for testing and to make sure they have appropriate training in place
- With your client’s consent, you can note in the file that he is trans, the name he prefers to be called (if different from the name on his health card) and his preferred gender pronouns (often he, him, they and their).
Cervical cancer screening
Use the diagram below to find out what type of cervical cancer screening is recommended.

- Gauge your client’s comfort with the exam. Some, but not all, trans men may feel uncomfortable with the idea of penetration and may feel their gender is undermined by the function of the speculum. It may be helpful to explain why a speculum is needed.
- Ask if a client has had a Pap test before, or whether he has had vaginally penetrative/frontal sex. If a client has no experience with penetration, it may be helpful to know this in advance and to suggest that he try penetration at home first using a small toy, fingers or a speculum. This may help make the screening process less confusing or disturbing. Some trans men may be willing to try this, while others will not.
- Some trans men who are taking testosterone wil have fewer secretions, so using lubrication and warm water can be helpful in speculum insertion. If lubrication is used, remember to record on the requisition.
- Testosterone can cause cervical cell changes that may make a trans man’s sample more difficult to read as it can mimic dysplasia. If the patient is on testosterone, note this on the requisition.
Ovarian cancer
Analogous to cis women with elevated androgen levels, testosterone therapy in trans men may increase the risk of ovarian cancer, although evidence for this is limited. There have been a few cases of ovarian cancer in transgender men 1 but no long-term studies exist. Overall the evidence regarding the risk of ovarian cancer in trans men on testosterone is inconclusive.2 Though evidence for their benefit in screening for ovarian cancer is limited, annual bimanual exam can be considered if ovaries are present, in accordance with the provider’s routine practice with cis women.
Sources
- Mueller A, Gooren L. Hormone-related tumors in transsexuals receiving treatment with cross-sex hormones. Eur J Endocrinol. 2008; 159(3):197-202.
- Feldman J and Safer J. 2009. Hormone Therapy in Adults: Suggested Revisions to the Sixth Version of the Standards of Care , Intl J of Transgenderism. 2009; 11(3)146-182, DOI: 10.1080/15532730903383757