Initial assessment tasks
The following is a guide to the assessment process with new (or newly transitioning) trans clients who have reached tanner stage V in pubertal development and are interested in hormone therapy. It is more important that the tasks of the assessment period are completed, rather than a certain number of visits logged or period of time elapsed.
Download assessment checklistCriteria for Hormone Therapy
- Diagnosis of Gender Dysphoria (according to the DSM-V-TR)
- Psychosocial readiness to begin treatment
- Completion of a period of assessment including appropriate physical and laboratory investigations
- Absence of absolute contraindications
- Optimal mitigation of risks relating to pre-existing health conditions
- Client understanding of risks, precautions and side effects of treatment
- Informed consent
- Harm Reduction
Client history
Rationale for assessment period
The assessment period is important for:
- Establishing rapport with the client
- Ensuring the client is ready
- Ensuring the client has all the information they need to start hormone therapy
Using respectful language
- Facilitate a trusting, open relationship by using respectful language.
- Always name your client by their chosen name and pronouns. If you are unsure, ask the client how they would like to be called.
- Use references that describe someone’s present identity (how they identify on that day), not their assigned identity.
- It is also helpful to check in with a client regularly about changes in their preferred name or pronouns and to encourage them to let you know if they change in the future.
Questions to ask:
How would you like to be addressed? What name and pronoun would you like me to use?

General medical intake & medical history
If this is a new client, attempt to get old records from previous provider(s)
Gender history
Speaking with clients about their history and experience with gender is not something that healthcare providers are typically taught during their training. It is, however, an important part of getting to know a trans client and informs the discussion around the development of an individualized care plan. Reassure your client that there are no ‘wrong answers’, nor any specific narrative that the provider is looking to hear. Not all trans people experience gender dysphoria or display gender non-conformity in childhood; trans identities may emerge at any point in the life cycle.
Click to view possible questions to open a conversation about gender identity

Baseline data
Vitals
Screening measures include blood pressure, height, weight, waist & abdo circumference
Focused Physical Exam
The physical exam, like the general periodic health exam, is used to rule out any dysfunction of a major body system and to offer opportunities to prevent and screen for disease.
Many trans clients have avoided medical practitioners because of fear of mistreatment or stigmatization, thus have often not had routine screening maneuvers employed. A discussion about risks and benefits of a particular manoeuvre may be helpful. In some situations an exam can be deferred to another time and/or refused.
You can build rapport and increase a client’s comfort by:
- Carefully explaining to the client ahead of time why the exam is essential to the client’s health
- Ask the client if they have certain terms they would prefer you to use to refer to specific body parts.
Do you have any words to describe specific body parts that you would like me to use?
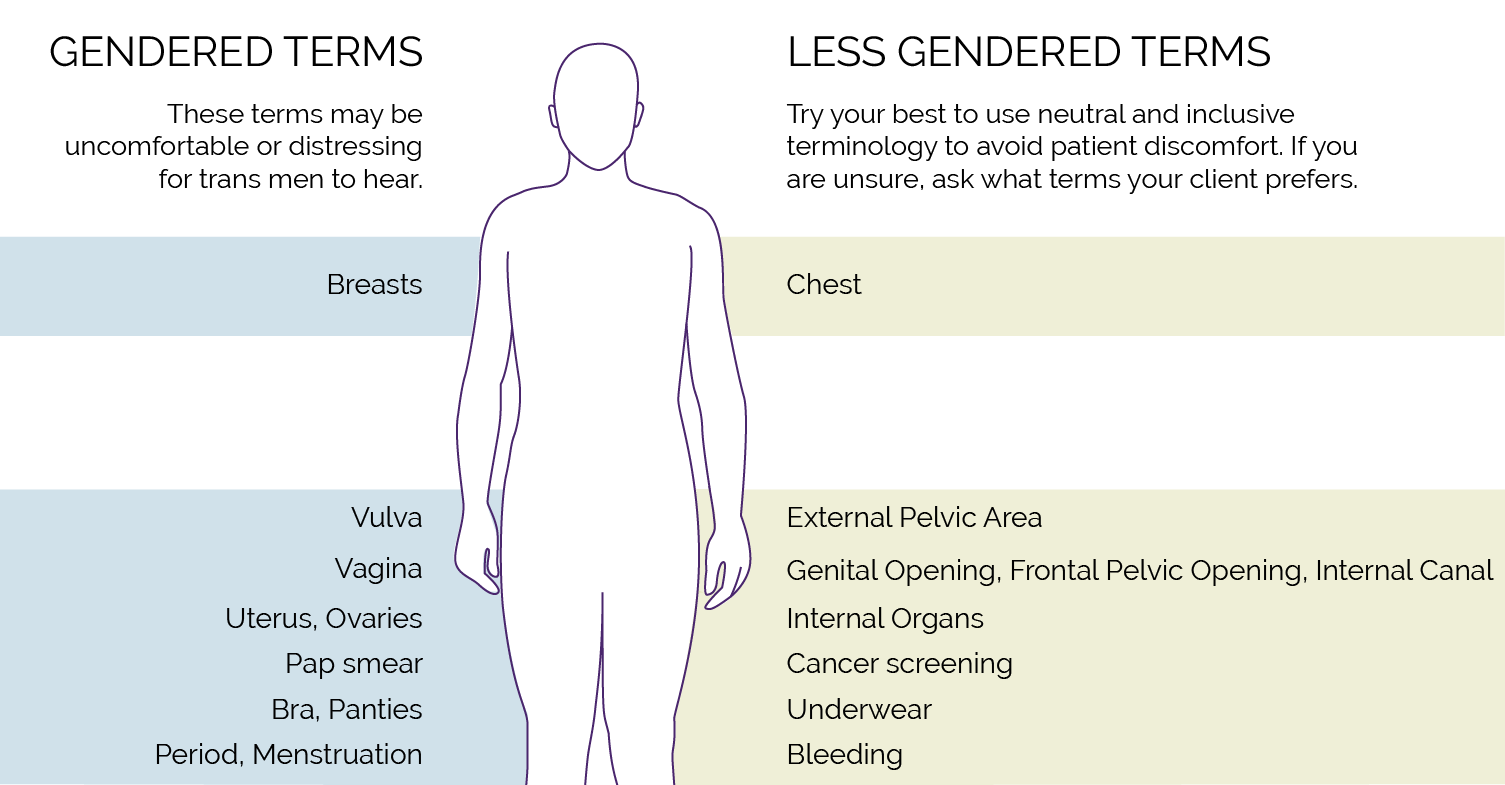
View suggested terminology to use for anatomy of trans men
Bloodwork
Laboratory tests should reveal any existing health problems such as liver dysfunction, high cholesterol, or diabetes. If present, these conditions should ideally be managed prior to starting hormones. The values will also provide a useful baseline to help with future monitoring for endocrine changes.
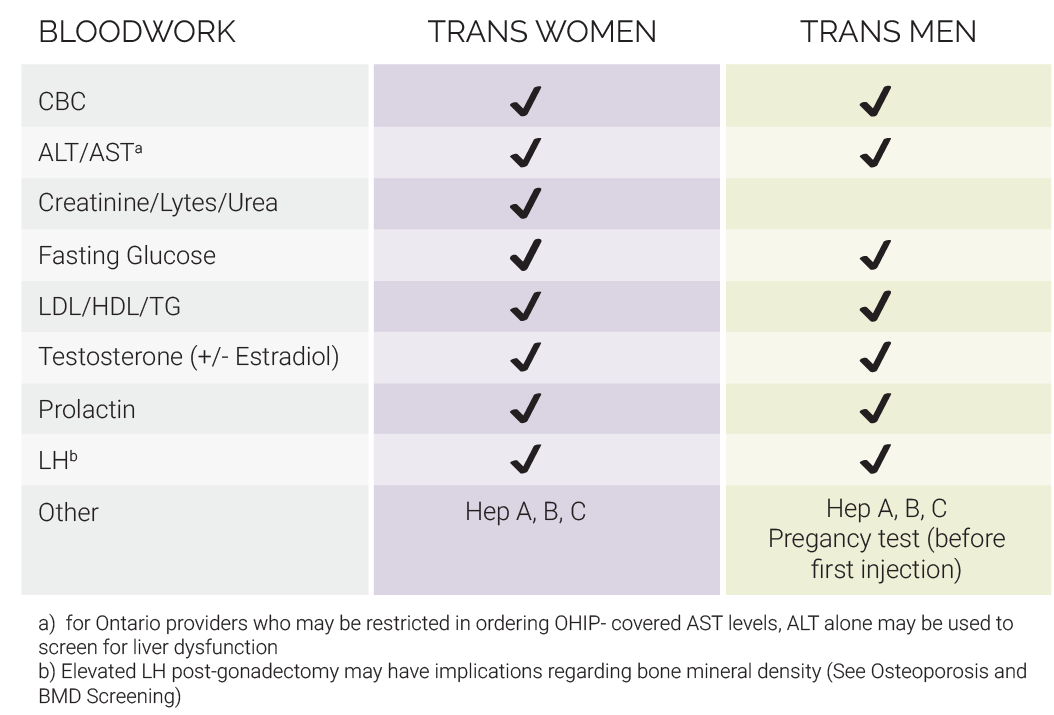
View baseline bloodwork summary for trans women and trans men
Health screening commenusrate to age & risk profile
An EKG should be completed if the client is over age 40, and a stress test should be considered if any additional risk factors for coronary artery disease are present.
Client education and readiness
Topics in this section:
-
Client's expectations
Fertility
Psychosocial supports
Advocacy
Potential benefits, risks and side effects
Capacity to consent
Medication options and costs
Ontario Drug Benefit
What are the client's physical transition goals?
Allow the client to articulate their transition goals.
Does the client have reasonable expectations?
Physical changes associated with hormones can be slow - it may take years to exhibit secondary sex characteristics. Underlying body structure for example will not change with hormones.
It may be helpful to provide the client with a copy of the estimated timelines for hormonal effects, while emphasizing that physiologic response to hormone therapy is highly individual.
Expected effects and timelines of feminizing hormone therapy
Expected effects and timelines of masculinizing hormone therapy
View possible questions to open a conversation about realistic expectations
Does the client hope to biologically parent a child one day?

Discuss the effects of hormone therapy on fertility with the client. Ask them whether they (and their partner) hope to biologically parent a child one day. If so, ask their interest in banking their sperm or eggs.
Options for preservation
Preservation options for trans women
If client suspects they may wish to have children in the future they should be advised to bank sperm prior to starting hormones.
Preservation options for trans men
Many trans men have become pregnant intentionally after discontinuing testosterone to pursue pregnancy. However, testosterone may affect fertility permanently. An option, although costly and potentially stressful, includes ova harvesting followed by ova or embryo cryopreservation. Associated costs are highly variable depending on the degree of ovarian stimulation required by the individual client.
Discuss the risk of pregnancy and options for contraception
Discuss pregnancy risk and options for contraception with the client. It’s important to have a discussion about sex and birth control.
View questions to open a conversation about sexual practice
Options for birth control
Birth control for trans women
Clients should be cautioned regarding the need for birth control if sexually active with partners who may become pregnant, since hormonal impact on fertility in trans women is variable.
Preservation options for trans men
Ask about the client's psychosocial supports
Gender transition can be a phase of significant adjustment in the life of the client. Like any major life stressor, the aim is to ensure the client has supports that facilitate healthy adjustment. When available, we recommend the client consider a support group setting (such as “Gender Journeys” or for youth: the LGBT youthline ).
The client may benefit from individual therapy with a trans-positive therapist with whom to discuss concerns about the transition process and to receive psychological support. Though not a requirement for the initiation of cross-gender hormone treatment, we encourage clients to discuss the transition with family members and friends as they too will have their own reactions and be affected by the client’s transition.
View possible questions to open a conversation about psychosocial readiness
Be an advocate for your client
Inquiring around how transitioning will influence the vocational or educational situation of the client is important, as providers can help the client develop strategies for dealing with gender change in school or the workplace. Unfortunately, it is not uncommon for transition to result in the loss of a job or struggle in the academic setting.
Common requests
Your client may seek assistance from you in order to access services and supports they may need. Below are some common support letters that primary care providers are frequently asked about.
-
Template Letter in Support of an Application For Change of Sex Designation on an Ontario Birth Registration
-
Template Letter in Support of an Application For Change of Sex Designation on an Ontario Driver’s License
Changes to gender markers on Ontario health cards
Sex designation will no longer displayed on Ontario health cards. Upon next renewal, cardholders will receive a card that does not indicate sex. If client wishes to get a health card without a sex indicator before their regular renewal date, they can get one by calling 1-866-532-3161 (TTY 1-800-387-5559) or by visiting any ServiceOntario centre. There is no fee to get a new health card.
Changes to gender markers on Ontario Driver's Liscence
In early 2017, driver's licence holders will be given the option to display an 'X' on their card as their gender identifier if they do not exclusively identify as male or female.
Potential benefits, risks and side effects associated with treatment
Discuss and ensure your client demonstrates a good understanding of the potential benefits, precautions and side effects of hormone therapy. Risks and precautions of the individual hormone treatments can be found in the feminizing and masculinizing hormone therapy section of this guide.
Does the client possess capacity to consent?
As with any other medical intervention, clients must demonstrate an understanding of the risks and benefits of hormone treatment. Obtaining informed consent is a process that primary care providers engage in daily, and when prescribing hormones to trans clients, the same basic principles apply. Questions may arise around capacity to consent in individuals with cognitive or development disabilities, mental health and substance use challenges, or younger clients. Sherbourne Health Centre implements an ‘informed consent model’ for hormone provision. In this model, the focus is on obtaining informed consent as the threshold for the initiation of hormone therapy, with less emphasis on meeting DSM diagnostic criteria for Gender Dysphoria or requiring a mental health assessment unless significant mental health concerns are identified.
-
Consent form for feminizing hormone therapy
-
Consent form for masculinizing hormone therapy
Review medication options with client
Discuss the different treatment options with the client. The formulations and recommended dosages of hormones can be found in the feminizing and masculinizing hormone therapy sections of this guide.
Discuss the potential costs of hormone therapy
Medication
Costs for medications vary and are listed in the feminizing and masculinizing Hormone Therapy sections.
Fertility
Fertility preservation is not presently covered by OHIP. Currently, some hospital-based clinics such as Mount Sinai Hospital’s Centre for Fertility and Reproductive Health, may offer a discounted rate for medically necessary gamete preservation and subsequent fertility treatment, such as in the case of gender transition. If indicated, referral to a fertility clinic should be initiated early in the hormone assessment period as this process takes time.
Hair Removal
Relevant especially to trans women since hormone administration may slow the growth of hair, it will not substantially reduce the amount of facial (or other body) hair that trans women possess. Laser treatments and/or electrolysis. These services are also not presently covered by OHIP and it can be a challenge to find a provider who is both sensitive to the trans client and able to work within fixed budgets. Permanently eliminating the bulk of facial hair may cost up to several thousand dollars and this should be discussed up-front and considered in the timeline of the client’s medical and social transition.
Submit Exceptional Access Program (EAP) for clients on Ontario Drug Benefit (ODB)
For clients covered by the Ontario Drug Benefit (ODB) program, oral estrogen (Estrace, Premarin) and intramuscular (IM) testosterone are covered with the submission of an Exceptional Access Form (EAP).
We suggest submitting the EAP application early in the process of assessment given that the processing time by the Ministry of Health and Long Term Care is variable and may take two months or more. Approval does not commit the provider to prescribing hormone therapy but prevents undue delays once the assessment period is complete.
-
Sample Request for an Unlisted Drug Product: Oral Estradiol
-
Sample Request for an Unlisted Drug Product: IM Testosterone
Risk management
Have precautions been optimally managed?
Ensure the absence of absolute contraindications to hormone therapy. Each hormone will have its own specific considerations and precautions which are explains in more details in the feminizing and masculinizing hormone therapy section of this guide. However, it is worthwhile to address general considerations and precautions with hormone use.
Lifestyle considerations
Smoking and obesity will increase the risks associated with hormone therapy. If the client smokes, smoking cessation counselling should be completed prior to hormone use. It is worthwhile for the provider and client to work to decrease these risks as much as possible, thus an exercise program, or smoking cessation program are recommended. Completion of these programs is not always feasible before starting treatment, and a harm reduction approach may be necessary. Substance use disorders – whether involving alcohol, illicit or prescription drugs – may introduce additional risks that should be considered. In the Toronto area, Rainbow Services at CAMH provides counselling and treatment services that are tailored to the needs of LGBT clients.
Mental health considerations
If present, psychiatric morbidity should be managed.
Although acute suicidality has previously been considered an absolute contraindication to hormone administration (particularly testosterone), there may be cases where a client who is at significant risk of suicide, but is able to provide informed consent, may in fact benefit greatly from the initiation of hormone therapy. This may be particularly true when intense gender dysphoria is the main source of the psychological distress experienced by the client. We suggest that these types of situations may be best approached on a case-by-case basis, with an assessment of the risks and benefits of hormone provision in relation to the individual client’s mental health. There may be situations in which the best course of action would be to start the client on low-dose therapy while strategizing around suicide risk reduction, for example by establishing a crisis plan and connecting the client with additional mental health support. If a client is experiencing a major depressive episode, pharmacotherapy for clinical depression should be discussed.
Differential diagnosis
Other possible diagnoses
Rule out other possible diagnosis (i.e. psychiatric disorders that could mimic gender dysphoria such as psychotic or dissociative disorders)
Does the client meet the Criteria for Gender Dysphoria?
The provision of hormone therapy is generally preceded by a diagnosis of Gender Dysphoria as outlined in the Diagnostic and Statistics Manual, Volume 5 (DSM-V-TR). There has been a great deal of debate in both the medical and trans communities around the appropriateness of using a psychiatric diagnosis for trans individuals. The recent revisions of the diagnosis (previously called Gender Identity Disorder) and associated diagnostic criteria in the DSM-V represent a step towards depathologizing gender difference and validating the spectrum of gender identity and expression. Certainly, there is potential for stigmatization and mistreatment of trans people if they are seen to have a psychiatric illness. However, there is also the ability to provide good care, make appropriate interventions, and guide research efforts based on the diagnosis. Thus, for many providers, the use of a psychiatric diagnosis is not meant as judgment or stigmatization of trans individuals, but as a tool to defend appropriate medical intervention and treatment.
View criteria for the DSM-V-TR diagnosis of Gender Dysphoria
Harm reduction: Fast-tracking through the assessment process
Provision of hormone treatment may be undertaken, in some cases, without definitively establishing a diagnosis of Gender Dysphoria or excluding other possible diagnoses. Situations that warrant a degree of ‘fast-tracking’ through the assessment period are for example:
- a client who is using illicit hormones already
- a client has marked distress regarding their gender presentation
- you know the client’s medical and/or gender history well prior to the client seeking hormone therapy
- if another knowledgeable provider has recently performed part or all of the assessment and the associated records are available for review or a conversation with the prior provider can be arranged, all tasks of the assessment period need not be repeated
Situations that warrant ‘fast-tracking’ through the hormone therapy assessment process